Why the INSPIRE Study is Needed:
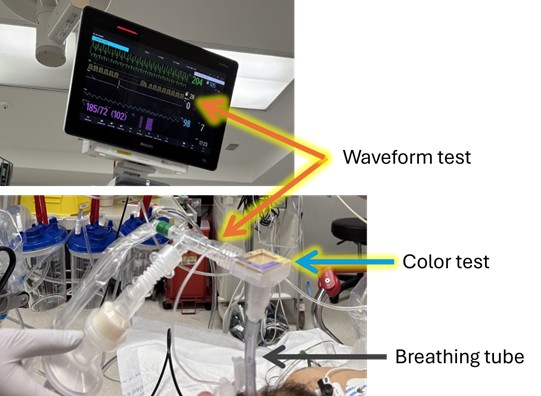
Each year millions of seriously ill adults need life-saving treatment with a breathing machine. To place someone on a breathing machine, doctors must place a breathing tube through the patient’s mouth and into the windpipe (a procedure known as “intubation”). When sick patients are placed on a breathing machine in an emergency department or intensive care unit (ICU), doctors commonly give patients a medicine to make them sleepy and comfortable (a “sedative”) while the breathing tube is being placed. Many doctors also give a second medication to temporarily immobilize the patient’s muscles to make it easier to place the breathing tube (a “neuromuscular blocker”). Which approach is best is uncertain.
Each approach has potential benefits and risks. Giving only a sedative may prevent low oxygen levels by allowing patients to continue breathing on their own during the procedure, but it might make it harder for doctors to place the breathing tube. Giving both a sedative and a neuromuscular blocker might make it easier for doctors to place the breathing tube, but it might lead some patients to feel awake but unable to move during or shortly after the procedure.
Patients who need a breathing machine are often seriously ill. Understanding which of these two approaches results in the best outcomes for patients is important.
What we are doing
We are doing a research study called “INtubation with Sedation Only to Preserve Independent Respiratory Effort” (INSPIRE). The goal of the study is to learn whether, for patients being placed on a breathing machine in an emergency room or ICU, using only a sedative or using both a sedative and a neuromuscular blocker is best for patients.
During the study, if doctors and nurses feel that using only a sedative would be best for a patient, they use only a sedative. If they feel that using both a sedative and a neuromuscular blocker would be best for a patient, they use both a sedative and neuromuscular blocker. If doctors and nurses do not have a feeling about which approach would be best for a patient, the patient is enrolled in the INSPIRE trial. For patients in the INSPIRE trial, a computer randomly assigns the patient either to receive only a sedative or to receive both a sedative and a neuromuscular blocker. This means every patient has a fair and equal chance of receiving either approach.
Consent for Emergency Care
Placing seriously ill adults on a breathing machine is an emergency procedure. There is often no time for doctors to discuss the risks and benefits of the procedure or the risk and benefits of the medications that will be used. Patients are often unconscious or too sick to make decisions. So, doctors go ahead with life-saving care without the patient’s okay (“consent”).
Consent for Research during Emergency Care
For these same reasons, it may not be possible to get patients’ consent for a study comparing use of only a sedative to use of both a sedative and a neuromuscular blocker. But important research to improve care for life-threatening conditions can sometimes be done without getting patients’ consent ahead of time. This is through a process called “Exception from Informed Consent Requirements for Emergency Research (EFIC).” Studies done with EFIC are designed with input from patients, families, and community members and overseen by an independent ethics committee.
If you were to be seriously ill and receiving a breathing tube in an emergency department or intensive care unit taking part in the INSPIRE study and your doctors determined that it would be safe to perform the procedure with either a sedative alone or both a sedative and neuromuscular blocker, you could be enrolled in the INSPIRE trial. You would receive whichever approach the computer randomly assigned to you. There might not be time to ask if you would like to take part in the study beforehand. But an INSPIRE study team member would come to you (or your family) after the procedure. They would tell you about the study, ask for your consent to continue participating in the study going forward, and provide information about how to stop taking part at any time, if you so choose.
Participating Sites
- Vanderbilt University Medical Center
Frequently Asked Questions
Who is eligible?
Adults who are receiving treatment in an emergency room or ICU whose doctors have determined that they need a breathing tube may be eligible for this study. Patients are only eligible if their doctors and nurses think that either strategy would be safe and effective. Patients can only participate if they are undergoing breathing tube placement at a hospital participating in the study. They cannot volunteer at any other time.
What are the risks of intubation with only a sedative?
Giving only a sedative may prevent low oxygen levels by allowing patients to continue breathing on their own during the procedure, but it might make it harder for doctors to place the breathing tub
What are the risks of intubation with a sedative and a neuromuscular blocker?
Giving both a sedative and a neuromuscular blocker might make it easier for doctors to place the breathing tube, but it might lead some patients to feel awake but unable to move during or shortly after the procedure.
Why are you sharing information about this trial with the community?
The goal of the INSPIRE trial is to produce information that helps patients, families, doctors, and nurses choose the approach that results in the best outcomes for patients receiving a breathing tube in the emergency room or ICU. Making sure that patients, families, and community members know about the study and its findings is important to achieving this goal. For that reason, patients, family members, and community members helped design the study, are helping to lead it, and will help us share the results of the study when it is completed. The results will be shared with the patients who participated in the study and with the community. We want people to be aware of the study, have an opportunity to ask questions, and have their voices heard.
How can I provide more feedback about the study?
We are interested in the community’s feedback about the study. Below is a link to a survey that asks specific questions related to the study: https://redcap.vumc.org/surveys/?s=J9KA7333PDW3RMKW